In recent years, the emphasis on improving medical outcomes in healthcare has significantly increased. Healthcare providers are now leveraging advanced technologies and evidence-based practices to enhance patient care. By focusing on medical outcomes in healthcare, institutions can better track patient progress, identify areas for improvement, and implement strategies that lead to better health results. This approach not only benefits patients but also helps in optimizing the overall efficiency of healthcare systems.

Operational Efficiency and Resource Optimization
AI technologies have the potential to optimize healthcare operations, reducing costs and enhancing efficiency. Intelligent automation can streamline administrative tasks, such as appointment scheduling and billing, allowing healthcare professionals to dedicate more time to patient care. AI-driven predictive analytics can also optimize resource allocation, forecasting patient inflows, optimizing bed management, and reducing wait times, ultimately enhancing patient satisfaction and productivity.
Clinical Decision Support and Error Reduction
AI algorithms can assist clinicians in making informed decisions by providing real-time insights and evidence-based recommendations. Natural Language Processing (NLP) algorithms can analyze unstructured data from clinical notes, research papers, and medical literature, helping physicians stay abreast of the latest medical advancements. AI-powered clinical decision support systems can analyze patient data, medical histories, and treatment guidelines, alerting healthcare providers to potential drug interactions, adverse events, or treatment options, thus reducing medical errors and improving patient safety.
Improving Medical Outcomes in Healthcare
In addition to advancements in technology and the adoption of evidence-based medicine, there is also a strong desire within the healthcare industry to optimize healthcare delivery. This involves streamlining processes, reducing inefficiencies, and improving coordination and communication among healthcare providers. By optimizing healthcare delivery, providers can ensure that patients receive timely and appropriate care, leading to improved outcomes. This may involve implementing electronic health records systems, utilizing telemedicine technologies, or implementing care coordination programs.
In conclusion, the focus on improving medical outcomes in healthcare is driven by a variety of factors, including advancements in medical technology, the adoption of evidence-based medicine, and a desire to optimize healthcare delivery. By harnessing these factors, healthcare providers can enhance patient care and ensure that individuals receive the best possible treatment and results. As the healthcare landscape continues to evolve, the importance of improving medical outcomes will remain a top priority for the industry.

AI-Driven Advancements in Patient Care
Personalized Treatment Plans and Precision Medicine
AI’s ability to analyze comprehensive patient health data, including genetics, medical history, lifestyle, and real-time health metrics, facilitates the creation of personalized treatment plans. By tailoring treatments to individual characteristics and predispositions, AI enhances the likelihood of treatment success, minimizing adverse effects and increasing treatment effectiveness. This personalized approach recognizes and respects the unique needs of various demographic groups, promoting inclusivity and addressing historical healthcare disparities, ultimately improving medical outcomes in healthcare.
Accelerated Drug Discovery and Development
AI is driving significant improvements in clinical trial design and optimization of drug manufacturing processes. AI-powered simulations facilitate the prediction of molecular interactions and the evaluation of potential drug effectiveness, substantially speeding up the research and development process for new medications. This is especially crucial for tackling diseases with limited treatment options. AI systems can analyze vast datasets to identify promising compounds for further investigation, ultimately reducing the time and resources required to bring new drugs to market.
Remote Healthcare and Telemedicine
AI-powered telemedicine and remote healthcare services have become more essential, particularly in remote or underserved regions. Telemedicine platforms allow patients to receive healthcare services from the convenience of their homes or local clinics, frequently utilizing AI-driven diagnostic tools and virtual consultations. This approach reduces barriers to healthcare access, including factors like geographic distance or inadequate healthcare infrastructure. AI plays a role in remote patient monitoring, wearable devices, and diagnostic tools, allowing healthcare professionals to remotely track patient vital signs and provide timely interventions when necessary, promoting healthcare equity and reducing the burden on healthcare facilities.
Successful AI Implementation in Healthcare
IBM Watson for Oncology
IBM Watson for Oncology is an innovative AI system designed to assist oncologists in making vital treatment decisions. By examining a vast repository of medical literature, clinical trial data, and patient records, Watson for Oncology delivers personalized treatment recommendations for cancer patients. This AI system takes into account various factors, including the patient’s medical history, genetics, and the latest medical research, helping oncologists choose the most appropriate and evidence-based treatment options.
Google Health's DeepMind
DeepMind, a branch of Google Health, has made substantial advancements in the healthcare field through its AI technology. In particular, DeepMind’s AI algorithms have been utilized for predicting patient deterioration.By examining patient data, including vital signs, lab results, and historical records, AI models can detect patterns and shifts that may signal patient decline. This early warning system enables clinicians to take proactive measures, potentially averting adverse events and enhancing patient safety.
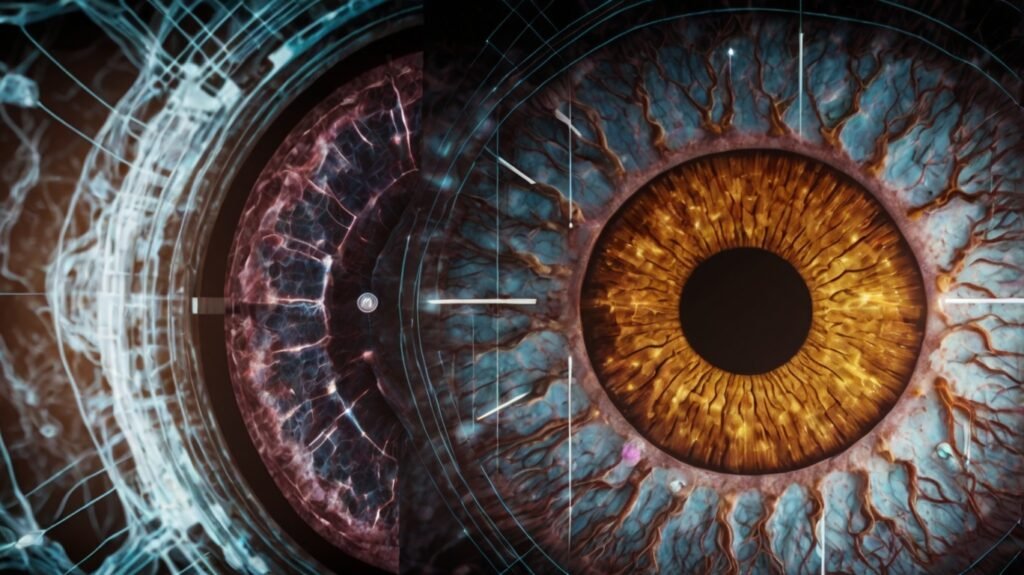
IDx-DR: AI-Powered Diabetic Retinopathy Detection
IDx-DR is an innovative AI-driven system that has gained FDA approval for the autonomous detection of diabetic retinopathy, a frequent diabetes complication that can result in vision loss if not addressed promptly. diagnosed and treated. This AI system analyzes retinal images and, with a high degree of accuracy, identifies the presence of diabetic retinopathy. By automating the diagnostic process, IDx-DR helps mitigate the shortage of eye care specialists in numerous areas and enables early detection and intervention, potentially preventing vision impairment in patients. Medical outcomes in healthcare are significantly improved with such technologies, ensuring better patient care and efficient resource utilization.

PathAI: AI-Driven Pathology Diagnostics
PathAI exemplifies the transformative power of AI in the field of pathology. Utilizing AI algorithms, PathAI aids pathologists in diagnosing diseases from histopathology slides with remarkable precision.. These algorithms can detect subtle and complex patterns in tissue samples, aiding pathologists in making more precise and timely diagnoses. This improves diagnostic precision and optimizes the pathology workflow, shortening the diagnosis time and facilitating quicker treatment decisions.
Addressing Healthcare Disparities with AI
AI holds immense potential in narrowing healthcare disparities and promoting equitable access to quality care. By leveraging AI’s capabilities in early detection, telemedicine, predictive analytics, and personalized medicine, healthcare providers can address longstanding barriers and ensure that advancements benefit all segments of society.
Enhancing Early Detection and Diagnosis
AI-driven algorithms can analyze vast amounts of medical data, identifying patterns and anomalies that might escape the human eye. This technology enables faster and more precise diagnoses, especially in underserved areas with limited access to healthcare resources. By tackling inequalities in early detection, AI can help create a more equitable healthcare system and enhance health outcomes for everyone.
Telemedicine and Remote Care
Telemedicine, augmented by AI, is a frontier in the quest for health equity. AI-driven remote consultations and diagnostic tools provide healthcare access to people in rural or economically disadvantaged regions. Patients who might have faced barriers in reaching healthcare facilities can now receive timely medical advice and interventions, reducing disparities in healthcare access and improving overall health outcomes.
Predictive Analytics and Preventive Care
AI-driven predictive analytics play a crucial role in preventive care. By analyzing population health data, AI can identify risk factors and trends, enabling healthcare providers to implement targeted interventions and education programs. This proactive strategy aids in preventing disease onset, easing the strain on healthcare systems, and ultimately enhancing health outcomes in various communities.
Addressing Language and Cultural Barriers
AI-powered language models and virtual assistants have the potential to bridge communication gaps in healthcare. These AI systems can provide information about risk factors, diagnoses, and treatment plans in a language and cultural context that patients can easily understand. By addressing language and cultural barriers, AI can increase patient literacy, promote adherence to treatment regimens, and ultimately improve health outcomes, particularly for disadvantaged populations.
Ethical Considerations and Challenges in AI Integration
Despite the immense potential of AI in healthcare, it is crucial to navigate its implementation with ethical considerations and address potential challenges to maximize its benefits while minimizing risks.
Data Privacy and Security
The utilization of AI in healthcare heavily relies on access to sensitive patient data, including medical records, diagnostic images, and genetic information. Safeguarding this information is paramount to maintaining patient trust and complying with healthcare regulations. Robust security measures, including encryption, access controls, and auditing, are vital to safeguard patient data against unauthorized access or breaches.
Algorithmic Bias and Fairness
AI algorithms can potentially inherit biases from the data they are trained on, leading to unfair or discriminatory decisions in healthcare. Addressing and mitigating these biases is a critical ethical concern. Healthcare organizations must meticulously curate training data to reduce bias, while AI developers should integrate bias detection and mitigation mechanisms into their systems. Regular audits and testing for bias in AI algorithms are essential to ensure fair and non-discriminatory healthcare decisions.
Transparency and Accountability
Ensuring transparency in AI algorithms is crucial to enable healthcare professionals and patients to understand the reasoning behind AI-driven recommendations. Healthcare organizations should prioritize the development of interpretable and explainable AI models, allowing for trust and informed decision-making. Clear guidelines for accountability should be established, defining the roles and responsibilities of healthcare professionals, AI developers, and organizations in cases of AI-related errors or adverse events.
Resource Constraints and Integration Challenges
Implementing AI systems in healthcare settings often requires substantial financial investment in technology and staff training. Smaller healthcare facilities may face challenges in allocating the necessary resources to adopt and maintain AI solutions. Overcoming this hurdle may involve seeking external funding partnerships, exploring cost-effective AI solutions tailored to specific needs, or gradual implementation to facilitate a smoother transition.
Collaborative Approaches and Future Prospects
To fully harness AI’s potential in healthcare, interdisciplinary collaboration, ethical guidelines, and the protection of patient rights are essential. Collaborative efforts among healthcare professionals, data scientists, engineers, policymakers, and technology developers are vital for driving AI-driven healthcare innovation while ensuring responsible and secure implementation. These combined efforts significantly impact Medical Outcomes in Healthcare by enhancing the quality, efficiency, and accuracy of patient care.
Interdisciplinary Research and Knowledge Sharing
Partnerships among healthcare professionals, data scientists, and engineers will be crucial in advancing AI’s impact in healthcare.Interdisciplinary research teams bring together diverse expertise to address complex healthcare challenges and improvemedical outcomes in healthcare. Open sharing of AI research, data, and models can accelerate progress and enhance the overall quality of AI applications in healthcare, fostering innovation and avoiding duplication of efforts.
Regulatory Frameworks and Policy Recommendations
Creating thorough and flexible regulatory frameworks is crucial for managing AI in healthcare. These frameworks should encompass guidelines for testing, validating, and approving AI applications in healthcare, defining requirements for AI safety, efficacy, data privacy, and ethical considerations. Flexibility is crucial to accommodate the rapid pace of AI innovation while ensuring patient safety and data security.
Patient Involvement and Empowerment
Involving patients in conversations about the role of AI in their healthcare is crucial for the successful implementation of AI. Patients should have a voice in decisions related to the use of AI in their care, including understanding how AI technologies work, obtaining informed consent for AI-driven procedures, and honoring patients’ choices regarding the use of AI in their healthcare. Patient-centered AI applications can lead to higher satisfaction, improved communication between patients and healthcare providers, and more effective healthcare delivery.
Continuous Education and Upskilling
Incorporating AI-related training into nursing and medical curricula is crucial for equipping healthcare professionals to efficiently utilize AI technologies. Healthcare education programs should include courses on AI fundamentals, data analysis, and practical applications of AI in healthcare, addressing ethical considerations and issues related to data privacy and bias. Ongoing education and upskilling opportunities will be crucial for healthcare professionals to stay updated on the latest AI advancements and ethical considerations, ensuring they can leverage these technologies to enhance patient care.
Conclusion: Embracing AI’s Transformative Potential
As we stand at the precipice of a healthcare revolution, the integration of AI holds immense promise in advancing diagnostics, treatment, and healthcare practices. However, realizing this transformative potential requires a collective effort from all stakeholders – healthcare professionals, researchers, policymakers, and technology developers – to navigate the complexities and challenges that accompany AI adoption.
By fostering interdisciplinary collaboration, establishing ethical guidelines, and prioritizing patient rights, we can harness AI’s capabilities to create a future where improved healthcare outcomes are not a privilege but a universal reality. The path ahead is not without obstacles, but by embracing AI’s transformative potential while upholding the highest standards of ethics and patient-centered care, we can propel the healthcare industry into a new era of precision, personalization, and equitable access to vital services.
